Journey to the origins of cancer: a survey of genetic changes that turn a healthy cell into a tumor cell
How does a normal cell become malignant? This question has been central to scientists and oncologists for many years, as it seems obvious that the response carries the solutions for the prevention, diagnosis and treatment of cancer.
One of the models chosen by Bertrand Nadel to study the causes of cancer is follicular lymphoma, a malignant tumor that develops from B cells, a subset of white blood cells that reside in part in the lymph nodes.
The role of B cells is to produce antibodies. These large proteins bind specifically to an antigen, that is to say, a fragment of a pathogen, that they then help to eliminate. B cells are produced continuously in the bone marrow as immature “naive” precursors, still unable to produce an antibody. They are first taught not to react against self (normal cells of the individual) and then circulate throughout the body, passing through various organs to become mature specialized cells (plasma cells and memory cells) capable of producing antibodies directed against a single antigen.
The genetic plasticity of B lymphocytes determines
their effectiveness but also their vulnerability!
Knowing that there are an infinite number of different pathogens, how can antibodies recognize as many specificities? The response of evolution to this formidable challenge resulted in a process of great virtuosity: change the genome of the cells both before and after the encounter with antigen. "The phases of the development of a naive B precursor into a plasma cell are governed by genetic mechanisms leading first to recombination of the genome (by rearranging genes relative to each other on the chromosome in millions of combinations), then a random transformation of these genes by mutagenesis," says Bertrand Nadel. "This 'plasticity' of intrinsic B lymphocyte chromosomes provides their incredible versatility, but makes them also very vulnerable: directed at the wrong time or wrong place, a change in the genetic code and/or the organization of genes may have dramatic effects for the cell. Lymphomas/leukemias associated with the subversion of such genetic modification programs are actually quite common, and follicular lymphoma is one of the most representative paradigms."
Evolution therefore naturally privileged efficiency - the immediate defense of the organism - to longevity, still constantly increasing in our societies.
A chromosomal aberration necessary or sufficient
for malignant transformation?
The translocation t(14; 18), the “hallmark” of follicular lymphoma, results from one of these errors. It creates a reciprocal exchange between chromosomes 14 and 18, which leads to an abnormal production of BCL2 onco-protein. When deregulated, this so-called "anti-apoptotic" molecule contributes to prolonged cell survival by reducing its ability to regulate itself and causes a cascade of secondary events leading to follicular lymphoma.
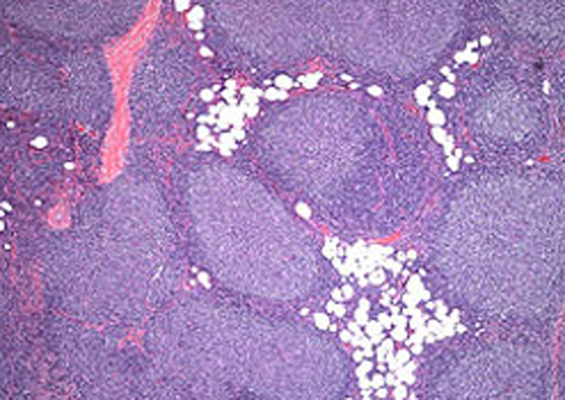
Follicular Lymphoma cells. Copyright hematologytimes.
"Although t(14;18) initiates lymphomagenesis, we and others have shown that 50-70% of healthy individuals carry a very small number of B cells with this translocation among their blood cells," says Bertrand Nadel. The frequency is however very variable and some individuals (approximately 1% of the population) have up to 1000 times more of these abnormal cells than the average, reaching a frequency close to that found in the blood of patients. "These B cells have other features that make them resemble follicular lymphoma: they persist for many years in the blood of individuals who bear them; they distribute in the lymphoid organs and are clonal, that is to say, originate from the duplication of a single original cell; they are abnormally blocked in their differentiation, and show an unusual instability of their genome."
These features are still not sufficient to transform B lymphocytes into lymphomas, but they put them at risk. Somehow, everything is set for the cell to become cancerous, so that a key “hit” turns the oncogenic switch: “recognizing and defining the moment at which this happens among the many progression steps of lymphomagenesis is our primary research goal”.
Early t(14; 18)+ precursors are thus probably still safe: what does it take for them to turn inexorably into tumor cells? How much time and how many other chromosomal alterations are needed? Which ones? In what order do they occur? Do environmental factors also come into play? These issues are central, since they potentially pave the way for new solutions for prevention, diagnosis or therapy.
Indeed, despite indisputable advances in recent years, follicular lymphoma (2nd adult lymphoma) is still regarded as incurable. Patients are often diagnosed late when the tumor burden is already high and the disease is frequently disseminated, particularly in the bone marrow. These patients are then treated with a combination of chemotherapy and targeted therapies, a heavy arsenal with dire side-effects.
If it turns out that the presence of some B cells carrying the t(14; 18) translocation indicate imminent occurrence of the disease, early diagnosis of these lymphomas could be considered in populations defined as "at risk". The identification of a predictive biomarker would have a major impact on public health, provided it is associated with an adapted therapeutic strategy, on the one hand taking advantage of "oncogenic flaws" present at early stages of tumor development, and on the other hand free of lasting side effects that are unacceptable for healthy individuals ("soft therapy").
"To reconstruct the sequence of events driving lymphomagenesis over such a period of time we have initiated major research programs, combining the expertise of epidemiologists,clinicians and biologists"
During malignant progression, oncogenic flaws are filled in; the tumor becomes more autonomous and gradually increases its ability to evade treatment. Early events that tip a normal cell into cancer are thus many control points (or rather, loss of control) that we may attempt to disrupt in order to block the process before it is too late. They thus represent excellent therapeutic targets for future drugs ... as far as one can decipher!
"Reconstructing the sequence of events driving lymphomagenesis and identifying key milestones is challenging, as it is currently technically very tricky to purify t(14; 18) B cells in 'healthy' individuals," says Bertrand Nadel. "Moreover, the complexity and heterogeneity of malignant progression coupled with the long latency preceding disease (it is estimated that follicular lymphoma may develop over several decades or even a lifetime!), require research programs of considerable scope and scale, combining the expertise of epidemiologists, clinicians and biologists."